BIOGRAFIA
___________________________________________________________________________________
Sergio Lima, ex-jogador profissional de futebol, natural de Campos dos Goytacazes, começou sua carreira no Americano FC, jogou em todas as categorias de base do clube. Em 1968 foi campeão campista juvenil, em seguida já com os profissionais em 1969, foi campeão Estadual. Ao finalizar o ano de 1969, Sergio foi transferido para o América do Rio.
______________________________________________________________________________________________
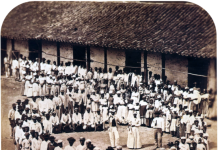
Em 1970, transferiu-se para o juvenil do América, ao final de 70 passou para os profissionais. Na sequência tornandou-se artilheiro da Taça Guanabara de 1973 e Vice-artilheiro do Campeonato Carioca de 1973. Atuou com extraordinários atletas Profissionais de futebol como, Edu, Thadeu Ricci, Jeremias, Sarão, Renato, Badeco, Alex, Luizinho, Gilmar, Ivo. Com o America foi Campeão da "TAÇA TAP" em 1973 importante torneio internacional realizado em Moçambique na África, tendo como adversário o gigante da época, o Benfica de Portugal e do craque Eusébio.
______________________________________________________________________________________________
Em 1974, sua história foi ilustrada luxuosamente com o Internacional de Porto Alegre, Hexacampeão Gaúcho invicto. Manga, Claudio, Figueiroa, Pontes, Vacarias, Paulo Roberto Falcão, Escurinho e Paulo Cesar Carpegiani, Valdomiro, Sergio Lima e Lula. Hexacampeão invicto.
______________________________________________________________________________________________
Em 1975, no Guarani de Campinas, formou um excelente time, com grandes jogadores, Ziza, Amaral, Renato, Miranda, Davi, Sergio Gomes, Estevão, Joãozinho, Voney, Bezerra, Alexandre Bueno, Edinaldo, Erb Rocha, Sergio Gomes, Hamilton, Rocha, Osnir, Dionísio. Este plantel que foi base do Campeão em 1978.
______________________________________________________________________________________________
Em 1976, transferiu-se para o futebol mexicano onde ficou por 8 anos: chegou no Club Jalísco, após o Clube Atlas Fútbol Clube ambos da cidade de Guadalajara, Morélia da cidade de Morélia, Michoacan e Union de Curtidores da cidade de Leon, Guanajuato. Em 1984, retornou ao Brasil para o Botafogo do Rio. Em 1985 foi contratado pelo Cabofriense, da cidade de Cabo Frio, estado do Rio, onde encerrou sua carreira.
___________________________________________________________________________________________
Presente em Guadalajara na Copa do Mundo 1986 no México, trabalhou como comentarista esportivo na Rádio local chamada “Canal 58” de Guadalajara. Após a Copa do Mundo de 1986, começou sua trajetória de 30 anos nos Estados Unidos da América, onde foi convidado pela Universidade de Houston, Texas, através do seu responsável o excelentíssimo Professor Franco, para participar como instrutor do “Cougar Soccer Summer Camp” durante duas semanas. Após finalizar o compromisso dos Soccer Camps com a Universidade, foi convidado por vários amigos mexicanos dirigentes de clubes amadores locais e resolveu ficar em Houston, Texas, e começar uma nova vida e carreira nos Estados Unidos.
______________________________________________________________________________________________
Na sequência, depois de várias participações em diferentes Soccer Camps no Texas, fundou, oficializou e legalizou a Brazilian Soccer Academy, com o apoio espetacular de um grande amigo americano Skip Belt. Com experiência de muitos anos dentro do campo, passou conhecimento e os fundamentos básicos do futebol do Brasil para um número incontável de jovens americanos.
______________________________________________________________________________________________
Convidado pelo consulado Mexicano, idealizou e apresentou o projeto Houston Soccer After School Program para City of Houston Park and Recreation em 1994, para benefício de crianças e jovens entre 6 a 17 anos. Isso ocorreu na área metropolitana da cidade, onde concentrava a grande maioria de crianças e jovens negros e mexicanos, na época estavam com extremo e grande problema social que os envolvia com drogas e as abomináveis gangues. Desafio aceito, e o programa foi desenhado, aproveitando a infraestrutura dos Parks da cidade. O passo a passo foi dividido em três fases básicas:
______________________________________________________________________________________________
1 – Criou-se uma liga em cada Park, onde havia jogos entre eles.
______________________________________________________________________________________________
2 – Todos os meses havia torneios entre todos os Parks.
______________________________________________________________________________________________
3 – Criou-se seleções para jogarem contra jovens de outras áreas e diferentes estados, sempre cuidando com os mínimos detalhes dos dispositivos e ensinamentos básicos do respeitado futebol do Brasil, para atrair e motivar a todos. O requisito principal era estar e manter boas notas e presença na escola, para desfrutar dos benefícios, recebendo gratuitamente todos os materiais de primeira linha doados por um conhecido patrocinador. Finalmente, aos 17 anos tinham a oportunidade de receber uma bolsa de estudos para ingressar em uma universidade americana.
______________________________________________________________________________________________
Foi apresentado e aprovado, Sergio se transformou em funcionário público da cidade de Houston por 17 anos até a sua aposentadoria. Muitíssimos jovens foram beneficiados pelo programa mudando radicalmente suas vidas, as drogas e gangues desapareceram.
______________________________________________________________________________________________
Sergio fez o curso de treinador da Federação Americana de Futebol, recebendo a “Licença National B’ e assumiu como Coach principal da Seleção do Sul do Estado do Texas, "South Texas Soccer Select Team Open Age". From 1994 to 1996, tornando-se o primeiro treinador brasileiro e negro “Afrodescendente” a dirigir a Seleção do Sul do Estado do Texas.
___________________________________________________________________________________________
Em 7 de setembro de 1992, fundou o Jornal Vida Brasil Texas, tornou-se editor, onde está até hoje maio de 2025, prestando este serviço a comunidade há 32 anos. O Jornal impresso foi até 2016 e os últimos 9 anos digital em português.
______________________________________________________________________________________________
Fundou em 2004, a Revista Brazilian Texas Magazine, é seu Editor. A revista até 2015 foi impressa, em 2016, passou a publicação digital em inglês.
______________________________________________________________________________________________
Compositor, teve participação do CD Brasil Forever 1997 da Banda brasileira criada no Texas em 1993, com finalidade de promover a cultura do Brasil. A Banda “Atravessados de Houston” – Texas, com tiragem de 10 mil CDs. Sergio Lima teve a participação com 10 músicas, sendo 8 autorais e 2 com parcerias.
______________________________________________________________________________________________
Compositor da música “I Love Rio”, escrita em inglês em homenagem ao Rio de Janeiro, com a luxuosa interpretação da excelente Elícia Oliveira em inglês.
______________________________________________________________________________________________
(Está disponível no YouTube)
https://www.youtube.com/watch?v=l39hfwOkyYU&t=18s
_____________________________________________________________________________________________
Representou a comunidade brasileira do Texas na I Conferência “Brasileiros no Mundo”, realizada em maio de 2008, com uma extrema característica acadêmica. Local, Palácio Itamaraty, no Rio de Janeiro, de iniciativa da Fundação Alexandre de Gusmão – FUNAG, órgão ligado ao Ministério das Relações Exteriores – MRE.
______________________________________________________________________________________________
A II Conferência “Brasileiros no Mundo”, realizada em outubro 2009, se desenvolveu com uma acentuada conotação política, tornando em certos momentos o diálogo tenso, desconfortável e até certo ponto cansativo, devido a falta de elasticidade de algumas lideranças acostumadas, creio a pontuar e determinar o rumo das conversas e decisões, em suas áreas ou comunidades no Palácio Itamaraty, no Rio de Janeiro, de iniciativa da Fundação Alexandre de Gusmão – FUNAG, órgão ligado ao Ministério das Relações Exteriores – MRE.
______________________________________________________________________________________________
Sergio criou o espaço Brasil, especial na Biblioteca central da cidade de Houston, conseguiu doações de livros de algumas instituições das comunidades brasileiras de outros estados americanos para compor o espaço.
______________________________________________________________________________________________
Recebeu o Prêmio Brazilian International PRESS AWARDS , por 3 vezes, em reconhecimento pelos trabalhos como editor do Jornal Vida Brasil Texas em português e revista Brazilian Texas Magazine em inglês – 2011.
ORIGINAL ARTICLE “AFRODESCENDENTES NA MÍDIA BRASILEIRA”.
______________________________________________________________________________________________
You are a winner for the 15th Annual Brazilian International PRESS AWARDS. Your outstanding performance and contribution for the Brazilian Culture was recognized by the Media and Cultural Leaders of the Brazilian Community in the United States. Join us for the 15th celebration of the Brazilian Cultural presence in the U.S.
______________________________________________________________________________________________
The Award Ceremony will be held at the Cinema Paradiso • Fort Lauderdale May 3rd 2012.
 By Kristi Rosa
By Kristi Rosa